Connect With Us
Blog

Foot Problems Related to Diabetes

Diabetic patients often face foot problems due to poor circulation and nerve damage, which may lead to numbness, tingling, or loss of feeling in the feet. This nerve damage, known as diabetic neuropathy, makes it harder to detect injuries like blisters, cuts, or pressure sores. Even small wounds can develop into serious infections if left untreated, especially when blood flow is reduced. In some cases, infections may become so severe that surgery is needed to remove affected tissue. Diabetes can also lead to structural foot changes, including Charcot’s foot, where weakened bones shift or break, resulting in deformity. If deformities occur, shoes may not fit properly, increasing the risk of skin breakdown. Regular evaluation by a podiatrist is important to monitor circulation, detect changes in foot structure, and prevent ulcers. A podiatrist can also provide appropriate footwear, custom inserts, or surgical correction, if needed. If you have foot pain that may be related to diabetes, it is suggested that you schedule regular appointments with a podiatrist for ongoing foot care.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Manisha Mehta, DPM from Detroit, MI. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Detroit, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
Wound Healing in Diabetic Patients

Wound healing in diabetics is often slower and more complex due to several factors. High blood sugar levels can impair circulation, limiting the delivery of oxygen and nutrients needed for tissue repair. Diabetes also affects the immune system, reducing the body’s ability to fight infection and respond to injury. Even small wounds, especially on the feet, can become serious if not treated promptly. Complications such as ulcers, infections, and in severe cases, tissue death may occur. A podiatrist plays a vital role in monitoring foot health, managing wounds, and preventing complications. They provide regular assessments, specialized care, and education on proper foot hygiene, footwear, and lifestyle habits. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you with proper wound care, in addition to managing this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Manisha Mehta, DPM from Detroit, MI. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Detroit, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
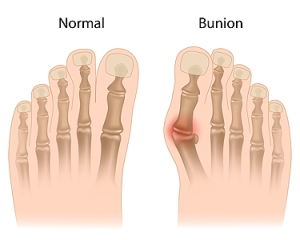
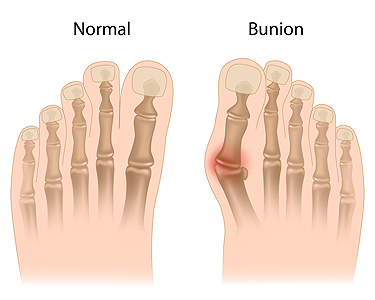
Bunions and Their Causes
A bunion is a bony bump that forms at the base of the big toe, causing the joint to stick out as the tip of the toe leans toward the others. Symptoms often include swelling, pain, redness, and difficulty wearing certain shoes. Bunions develop over time due to pressure on the joint, often caused by improper footwear, inherited foot structure, or arthritis. Risk factors include wearing narrow shoes, standing for long periods, and a family history of bunions. A podiatrist can evaluate the severity of the bunion, recommend supportive footwear, provide custom orthotics, and offer treatment options to reduce pain, improve alignment, and prevent the condition from worsening. If you notice the beginning signs of a bunion developing, it is suggested that you consult a podiatrist who can offer effective relief and treatment solutions.
If you are suffering from bunion pain, contact Manisha Mehta, DPM of Detroit, MI. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Detroit, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Symptoms of Stress Fractures

A foot stress fracture is a hairline crack in a bone caused by repeated pressure, often seen in the toes, midfoot, or heel. Pain usually begins gradually and worsens during activities like walking or running. It is often felt in one specific area and may seem mild at first, leading many people to ignore it. Unlike other injuries, a stress fracture may not cause swelling or bruising, making it even harder to recognize. As the fracture becomes more severe, the pain may become sharp and limit daily movement. A podiatrist can evaluate the injury by using imaging tests and may recommend a period of offloading. This means reducing weight placed on the injured area to give the bone time to heal. Offloading may involve using crutches, a walking boot, or limiting movement. In some cases, surgery may be needed if the fracture does not heal properly. If you experience symptoms of a stress fracture, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Manisha Mehta, DPM from Detroit, MI. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Detroit, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
What Is a High Ankle Sprain?

A high ankle sprain occurs when the ligaments above the ankle that connect the two bones in your lower leg, the tibia and fibula, are stretched or torn. This type of sprain is less common but often more severe than an ankle sprain that affects the ligaments surrounding the ankle joint. High ankle sprains are usually caused by a twisting injury or direct impact, often seen in sports like football, basketball, or skiing. Symptoms include pain above the ankle, swelling, bruising, and difficulty walking or bearing weight on the affected foot. The pain is often sharp and may worsen with activity or when the foot is rotated. A podiatrist can evaluate the severity of the sprain through a physical exam and imaging, offering treatments such as rest, elevation, immobilization, and, in some cases, targeted exercises. In more severe cases, surgery may be required. If you have a painful ankle sprain, it is suggested that you promptly schedule an appointment with a podiatrist.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Manisha Mehta, DPM from Detroit, MI. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Detroit, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022